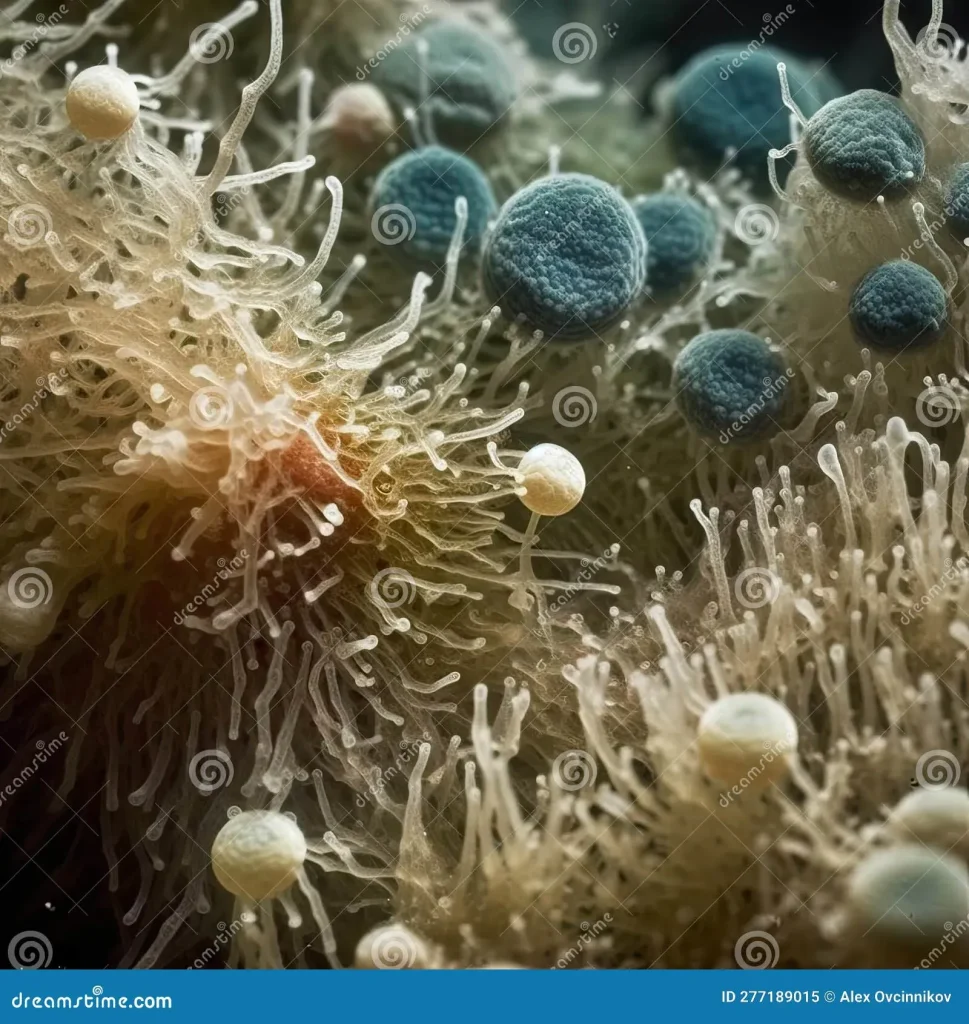
Candida auris has emerged as a drug-resistant fungus threatening patients in healthcare settings. Its ability to resist many antifungal medicines raises concerns about treatment options and patient outcomes. Candida auris infection cases have been linked to serious complications and longer hospital stays. The pathogen can persist on surfaces and spread between patients, amplifying the risk of outbreaks. Healthcare facilities worldwide are urged to strengthen infection control as it continues to challenge standard disinfection protocols.
Experts describe this organism as an emerging fungal pathogen that thrives in clinical environments. Its multi-drug tolerance adds risk for vulnerable patients and underscores broader concerns about drug resistance. Public health authorities are leaning on heightened surveillance and strict infection-control practices to reduce hospital-acquired infections. In the UK, the notifiable infection UK status is used to track outbreaks and coordinate a timely response.
Candida auris: A drug-resistant fungus threatening hospital patients
Candida auris (C. auris) has emerged as a drug-resistant fungus that poses a serious threat to patients in hospital settings. The World Health Organization highlights C. auris among the fungi of critical priority due to antifungal resistance, making infections hard to treat and control. This resilience aligns with the broader pattern of antifungal resistance driven by overuse of medicines in both healthcare and agricultural contexts, complicating efforts to keep hospital-acquired infections in check.
In recent clinical cases, including severe brain infections after traumatic injuries, C. auris can persist on surfaces and skin, potentially spreading despite standard cleaning. Healthcare teams must implement rigorous infection-control measures to prevent nosocomial transmission, particularly in intensive care units where vulnerable patients are at greatest risk. The combination of environmental persistence and limited effective therapies underscores why many health authorities describe C. auris as a formidable public health challenge.
How Candida auris infection spreads in healthcare settings
Candida auris infections can spread within hospital environments through contaminated surfaces, medical devices, and person-to-person contact, contributing to hospital-acquired infections. The organism’s ability to survive on inanimate surfaces for extended periods makes strict cleaning protocols and environmental decontamination essential components of outbreak prevention.
Accurate detection is crucial because misdiagnosis can delay targeted antifungal therapy and containment efforts. Given the limited arsenal of antifungal drugs and rising antifungal resistance, early identification and appropriate treatment are key to reducing transmission, protecting other patients, and slowing the spread of resistant strains within healthcare facilities.
Global impact, mortality, and risk factors of Candida auris
Candida auris infection has been linked to fatalities around the world, with some outbreaks showing high mortality rates. Its emergence is closely tied to antifungal resistance, a trend driven by overuse of antifungal medications and gaps in antimicrobial stewardship across regions.
People with weakened immune systems, recent healthcare abroad, prolonged hospital or ICU stays, or prior exposure to antibiotics are at higher risk for C. auris infection. These vulnerabilities, combined with environmental persistence and resistance patterns, contribute to the global spread and clinical impact of this notifiable and increasingly problematic pathogen.
Treatment challenges and evolving antifungal resistance in Candida auris
The traditional toolbox of antifungal medicines is proving insufficient against Candida auris, reflecting a broader pattern of drug-resistant fungi. C. auris is widely regarded as a critical priority pathogen due to rising antifungal resistance, which narrows effective treatment options and complicates clinical management.
Clinical experience shows that management may require complex regimens, sometimes combining multiple antifungal agents and extended therapy to achieve clearance. This ongoing resistance emphasizes the need for antimicrobial stewardship, ongoing surveillance, and the development of new therapeutics to outpace evolving strains.
UK response to Candida auris: Notifiable infection status and outbreak control
In the UK, Candida auris is a notifiable infection, meaning all cases must be reported to health authorities to help track and contain outbreaks. This requirement enhances surveillance and supports rapid public health action to prevent wider transmission within hospitals and communities.
Enhanced reporting and cross-institution coordination enable earlier interventions, isolation when needed, and targeted infection-control measures. The notifiable infection UK framework also informs international collaboration to curb cross-border spread of drug-resistant pathogens and to protect vulnerable populations from hospital-acquired infections.
Preventing hospital-acquired infections: lessons from Candida auris
Candida auris illustrates why stringent infection-prevention practices are essential in hospitals, including rigorous cleaning, effective surface disinfection, and consistent hand hygiene. The organism’s ability to persist on surfaces and skin heightens the risk of hospital-acquired infections when controls falter.
Proactive strategies—such as targeted screening for high-risk patients, appropriate isolation, staff education, and antimicrobial stewardship—are critical to stopping outbreaks. Ongoing public health guidance emphasizes surveillance, prudent antifungal use, and continuous monitoring to mitigate antifungal resistance and reduce the burden of C. auris in healthcare facilities.
Frequently Asked Questions
What is Candida auris infection and why is it described as a drug-resistant fungus?
Candida auris infection refers to infections caused by the Candida auris fungus, which has emerged as a drug-resistant fungus in many settings. The World Health Organization has called C. auris one of the deadliest fungi because it often resists the limited medicines available for treatment, and it can survive on hospital surfaces and skin for long periods, increasing transmission risk in healthcare facilities.
How does Candida auris infection relate to hospital-acquired infections?
Candida auris infection is commonly linked to hospital-acquired infections. It can spread in hospital environments, persist on surfaces, and resist common disinfectants, making it possible to pass between patients and healthcare workers if strict infection-control practices are not followed.
What does antifungal resistance mean for patients with Candida auris infection?
Antifungal resistance means that standard drugs may be less effective against Candida auris infection. This resistance contributes to longer treatments, more complex care, and in some cases a higher risk of serious outcomes, underscoring the global concern over antifungal resistance in this pathogen.
Why is Candida auris infection a notifiable infection in the UK?
In the UK, Candida auris infection is a notifiable infection, meaning all confirmed cases must be reported to health authorities to help control outbreaks and protect vulnerable patients by enabling timely surveillance and response.
How is a Candida auris infection diagnosed and treated in a hospital setting?
Diagnosis typically involves microbiological testing to identify Candida auris. Treatment in the reported case included three weeks of antifungal injections, followed by two antifungal drugs administered via IV for 15 days, and an 11-day course of oral antifungal tablets, with blood tests confirming clearance before discharge.
Who is at higher risk for a Candida auris infection?
People with weakened immune systems, those who have recently received healthcare abroad, patients with long hospital or intensive care stays, or those treated with certain antibiotics are at higher risk for Candida auris infection and subsequent antifungal resistance.
Why is Candida auris considered a serious global threat by public health organizations?
Candida auris is highlighted as a serious threat because it is a drug-resistant fungus that can cause hard-to-treat infections, spread in healthcare settings, and has been identified among the fungi in WHO’s critical priority group, indicating urgent research and containment needs.
What preventive measures are important to reduce Candida auris hospital-acquired infections?
Prevention focuses on robust infection-control practices in healthcare settings, vigilant cleaning to counter persistence on surfaces, early identification of cases, and prompt isolation where appropriate to limit the spread of Candida auris infection.
What types of infections can Candida auris cause if it spreads in the body?
Candida auris can spread to multiple sites, including the blood, brain, spinal cord, bones, abdomen, ears, lungs, and urinary system, leading to a range of serious hospital-acquired infection symptoms that require urgent medical care.
What did the WHO’s priority group include that mentions Candida auris, and why does that matter?
The WHO’s critical priority group includes four fungi: Aspergillus fumigatus, Candida albicans, Cryptococcus neoformans, and Candida auris. This designation underscores the urgent need to monitor, prevent, and treat infections caused by these high-priority fungi, including Candida auris.
How does antifungal resistance develop, and what role can agriculture play in this trend?
Antifungal resistance develops through the overuse and misuse of antifungal medicines. The case notes that excessive use of antifungal agents in agriculture and healthcare contributes to resistance in Candida auris, highlighting the broader impact of over-the-counter access and agricultural practices on public health.
If a healthcare provider suspects a Candida auris infection, what steps should be taken in the UK?
Suspected cases should be tested to confirm Candida auris infection, with appropriate reporting to health authorities as required by the notifiable infection UK status. Implementing infection-control measures and coordinating with public health authorities helps prevent outbreaks and protect patients.
| Key Point | Details |
|---|---|
| What is Candida auris? | A drug‑resistant fungus identified in 2009; WHO calls it a serious threat. It can survive on hospital surfaces, spread in healthcare settings, and cause infections in blood, brain, spinal cord, bones, abdomen, ears, lungs and urinary system; associated with deaths and a fatality rate around 1 in 3. |
| WHO priority group and global threat | Candida auris is one of four fungi in WHO’s critical priority group (alongside Aspergillus fumigatus, Candida albicans, Cryptococcus neoformans). The fungus is spreading in hospitals worldwide and remains difficult to treat due to antifungal resistance. |
| Recent UAE case overview | A 34-year-old man developed C. auris infection about 99 days into hospitalization after a traumatic brain injury from a car crash. He underwent emergency brain surgery, spent weeks in ICU, had multiple procedures and antibiotics, and was discharged after seven months with the infection eliminated. |
| Transmission and resistance traits | C. auris can persist on hospital surfaces and is often resistant to disinfectants and many medications; it can spread to the blood, brain, spinal cord, bones, abdomen, ears, lungs and urinary system. |
| Treatment course in the UAE case | The patient received three weeks of antifungal injections, two drugs via IV for 15 days, and an 11‑day course of antifungal tablets. Blood tests later cleared, and he was discharged after seven months. |
| Risk factors | Weakened immune systems, recent healthcare abroad, long hospital/ICU stays, or prior antibiotic treatments increase risk. |
| UK/notifiable status and outbreak control | In the UK, Candida auris is a notifiable infection, meaning all cases must be reported to help control outbreaks. |
| Drivers of resistance and broader context | Widespread antifungal use in healthcare and agriculture, plus over‑the‑counter availability in some developing countries, fuels antifungal resistance and makes most fungal infections harder to treat. |
Summary
Conclusion: Candida auris is a drug-resistant fungus that poses a growing global health threat in hospitals and care facilities. This organism can persist on surfaces and spread between patients, challenging infection control and treatment options due to its resistance to multiple antifungal medicines. The UAE case highlights the importance of robust infection prevention, early detection, and prudent antifungal use to prevent outbreaks. Notifiable reporting in regions like the UK helps track cases and coordinate responses to contain spread and reduce mortality associated with Candida auris.